Introduction
Oral health promotion services in Harrow are delivered by Whittington NHS Trust and the contract has been renewed for 2023-24.
The Health and Social Care Act (2012) conferred the responsibility for health improvement, including oral health improvement to local authorities and produced Commissioning Better Oral Health document to support with population – based interventions. Delivering Better Oral Health provides evidence-based interventions and advice on how dental health professionals can improve and maintain the oral and general health of their patients. The guidance is the result of a comprehensive review of published research evidence on prevention and draws on a UK wide collaboration of over 100 well respected experts including frontline dental teams and patient representatives. The guidance includes advice on how to prevent the main oral diseases dental caries, periodontal diseases, oral cancer and tooth wear with additional advice on:
- the use of fluoride
- brushing your teeth
- eating a healthy balanced diet
- how to support behaviour change
In 2021, the Whittington NHS Trust were commissioned to provide oral health promotion in Harrow. The approach follows the Marmot’s Review (‘Fair Society, Healthy Lives’) which recommends adopting proportionate universalism when developing strategies to improve health and reduce inequalities. This approach recommends actions that are universal, but with a scale and intensity that is proportionate to the level of disadvantage.
This approach acknowledges that concentrating solely on the most disadvantaged will not sufficiently reduce health inequalities. Applying the concept of proportionate universalism to oral health improvement for children means that a combination of universal and targeted activities is needed alongside specialist services. Everyone should receive some support through universal interventions, while children that are particularly vulnerable (e.g. looked-after children and children from families living in poverty), should receive additional interventions and support.
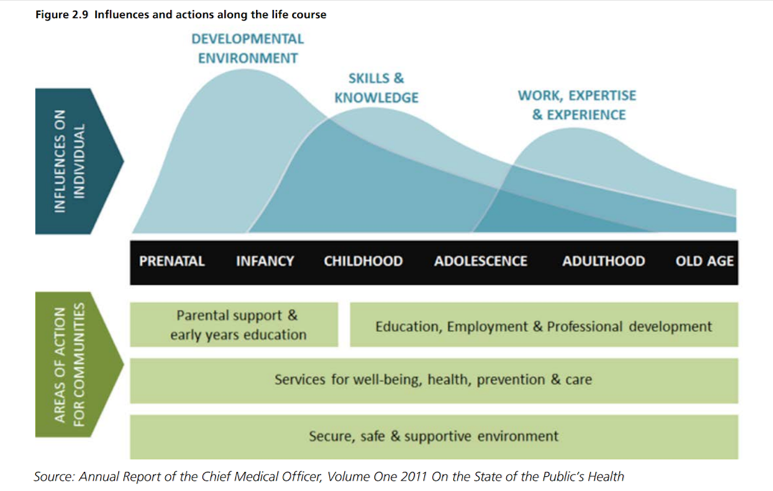
The Marmot Review and the public health white paper ‘Healthy lives, healthy people’ highlighted the importance of early life interventions in improving health and reducing avoidable health inequalities across the life course. This life course approach acknowledges that biological and social experiences throughout life have an impact on long-term health and wellbeing. The early years of a child’s life are critical to their future life chances because positive and negative effects accumulate throughout the life course. Adopting the life course approach allows the close links between early disadvantage and poor outcomes throughout life to be broken.
Influences and actions during the life course
Local Strategic priorities
Child oral health is a priority as part of Harrows health and wellbeing strategy. It is also a priority area for the 0-19 health visiting and school nursing service in Harrow.
Public health Harrow lead on a multi-agency steering group that meets quarterly to oversee activities related to promoting good oral health and dental hygiene amongst children and young people (0 -19/25 years with SEND) in Harrow. Key members include, 0-19 health visiting and school nursing, early support, early years education, the local dental committee, health improvement, dental oral health consultant OHID, community dental service and the voluntary and community sector, parent carer forum. The group is overseen by the health and wellbeing board. The aim of the steering group is to:
- To embed oral health practices using the principles of making every contact count.
- Align children’s oral health in all policies and reduce inequalities
- Mitigate A&E attendance for children needing extractions
- Facilitate partnership and multi-agency working and information sharing on children’s oral health at all levels highlighted in the Healthy Child Programme
- Facilitate and support oral health promotion training and skills development amongst practitioners and communities in Harrow in order to bring added value and consistency in messages given.
- Seek engagement of Harrow General Dental Practices through the Local Dental Committee particularly regarding access to referrals and appointments for children from 8months old
- Clear pathway for referrals by front line professionals and key workers for children where there is a concern
- Agree and recommend a series of measurable actions to improve children’s oral health in Harrow focussing on areas of need, vulnerable children and areas of high deprivation.
- Agree and recommend key messages for the public, dentists and other settings regarding children’s oral health and related services
- To monitor the implementation of agreed actions.
Child population
According to the GP registrations in Harrow, there is a population estimated at 290,963. The child population by age 0-5 is 19,265, and total 0-18 is 64,524. The number of children by age registered with a GP is shown in the table below.
Table 1: Children registered with a GP
| Age | GP registered pop |
| 0 | 2,747 |
| 1 | 3,217 |
| 2 | 3,184 |
| 3 | 3,350 |
| 4 | 3,366 |
| 5 | 3,401 |
| All 0-5 children | 19,265 |
| 6-11 | 20,871 |
| 12-18 | 24,388 |
| All children 0-18 | 64,524 |
Deprivation levels by ward in Harrow
Harrow is ranked 203rd out of 354 Districts in England where 1st is the most deprived. Harrow is less deprived in 2010, compared to 2007 when it was ranked 196th. Most multiple deprivation is in the centre of the borough, with pockets of deprivation in the south and east. Harrow’s least deprived areas are found in the west of the borough. Eight LSOAs in Harrow are in the bottom 10% nationally and the wards of Hatch End, Edgware, Marlborough and Harrow Weald each have a LSOA in the most deprived 5%. There are nine LSOAs in the least deprived 20% in the country, they are in the north-west (Pinner and Hatch End wards), north-east (Stanmore) and south (Harrow on the Hill). Headstone and Rayners Lane also have LSOAs in the least deprived 20% nationally.
Figure 1: Deprivation map in Harrow by ward
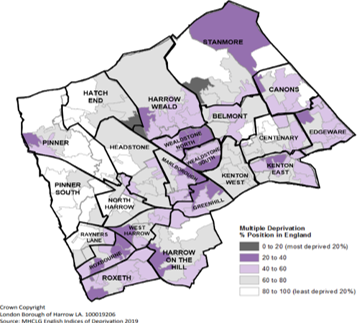
Wealdstone North and South, Marlborough, Greenhill, the north part of Stanmore and Roxbourne wards have the highest levels of deprivation in the borough.
Dental caries prevalence
The national dental epidemiology programme (NDEP) provides data on tooth decay experience among children. The survey is conducted every 3 years or so and seeks to survey children in schools. Key ages include surveys for 3 year olds, 5 year olds and 10-11 year olds.
Tooth decay experience in three-year-olds
The dental survey conducted in 3 year-old children in 2020 found Harrow to have a higher prevalence of experience of tooth decay (12.4%) when comparing it to England (10.7%). The prevalence of tooth decay experience in Harrow was similar to London (12.6%).
Table 4: prevalence of experience of tooth decay in three-year-old children
| Location | Prevalence of experience of tooth decay (%) in 3 year olds 2020 | Mean number of teeth with experience of tooth decay in children with any decay experience (95% confidence intervals) 2020 |
| Harrow | 12.4 | 3.3 (1.92-4.71) |
| London | 12.6 | 3.1 (2.85 – 3.32) |
| England | 10.7 | 2.9 (2.81 – 3.03) |
Tooth decay experience in five- year-olds
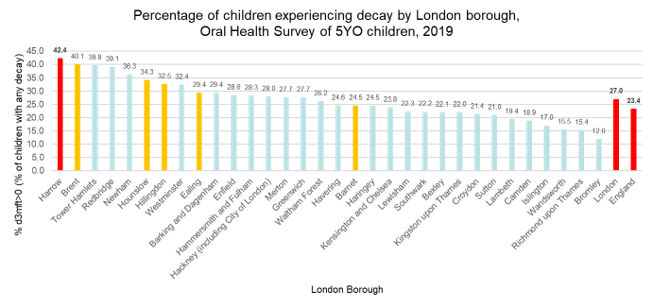
The dental epidemiology survey for 5 year olds in 2019 showed that 42.4% of children experienced tooth decay, the third highest compared to all Local Authorities in London. The prevalence of tooth decay experience in Harrow was higher than both London’s average (27.0) and England’s (23.4%). This increased from 39.6% in 2017.
Table 5: prevalence of experience of tooth decay in five-year-old children
| Location | Prevalence of experience of tooth decay (%) in 5 year olds | Mean number of teeth with experience of tooth decay in children with any decay experience (95% confidence intervals) |
| Harrow | 42.4 | 3.6 (3.04 – 4.66) |
| London | 27.0 | 3.4 (3.30 – 3.53) |
| England | 23.4 | 3.4 (3.36 – 3.44) |
Figure 2: Prevalence of experience of dental decay and mean number of teeth with experience of dental decay in 5-year-olds by local authority in London and England (Harrow is highlighted in red). Source: NDEP, 2019
The rate of hospital admissions related to dental caries for children (under 5) stands at 390 per 100,000 children under 5 for 2018/22 and consistently higher than London (280 per 100,000) and England (220 per 100,000) over time.
Local analysis indicates that there is a total of 342 admissions; more boys (179) have an hospital admission than girls (163).
Other White/ White British children account of the majority of all tooth decay admissions (35%, 116 children) followed by Asian (32%, 107), Mixed/Other (27%, 88 children) and Black children (6%, 20).
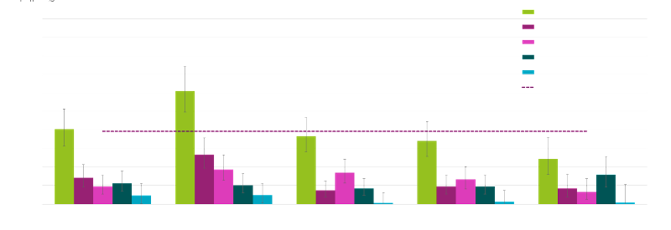
There is a socio-economic factor in tooth decay. Emergency admissions are almost 3 times more likely for children living in deprived areas (2nd most deprived), compared to affluent (610 per 100,000 vs 244 per 100,000). Mostly are Other White and Asian children (74%, 75 children).
Figure 3: Rate per 100,000 and number of hospital admissions related to dental caries by deprivation quintile and ethnicity, children aged 0-5, Harrow, 2018/22 (Source: WSIC primary and secondary dataset (March 2023) – NHS Dental Statistics of England (2023)
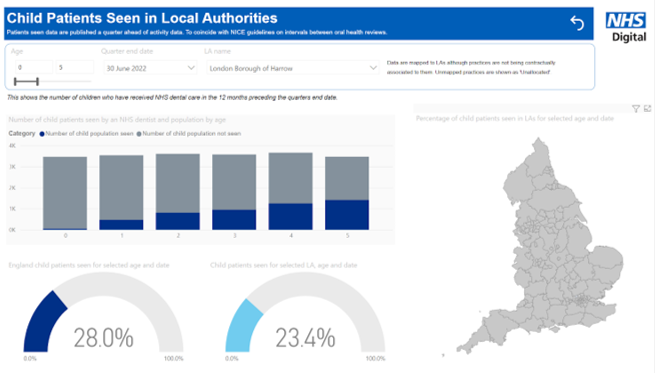
Dental Access
23.4% of children were seen in local dental surgeries in 2022, lower than the England average of 28%. As an approximate indicator, we can suggest that 65 to 70% of children do not access a dentist by the age of 5 years old. This highlights the importance of working with the community, front line services, schools and the early years sector so that oral health promotion targets the percentage of the population not seen by dentists.
Figure 4: Dental access in Harrow compared with England
Hospital admissions for dental extractions
The extraction rate for Finished Consultant Episodes (FCEs) for children and adolescents aged 0-19 admitted to hospital was higher in Harrow than London.
Figure 5: Number of Finished Consultant Episodes (FCEs) for children and adolescents aged 0-19 years admitted to hospital for extraction 2016 to 2021 by Local Authority, London Source: OHID, 2021.
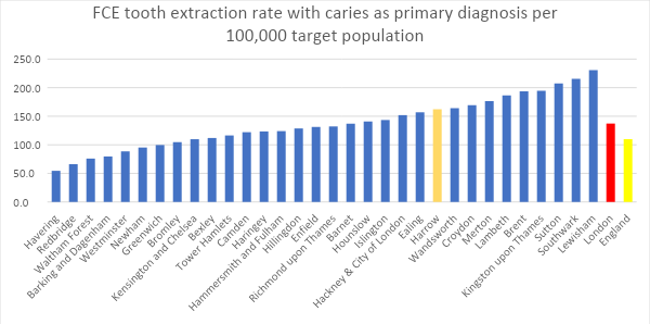
Note: There has been a 58.4% reduction in the number of episodes of caries-related tooth extractions in hospital for 0 to 19 year olds compared to the previous year, despite a 0.4% increase in the estimated population of this age group (across England). This is likely due to the continued impact of the COVID outbreak on non-COVID related hospital episodes, rather than sudden reduction in need or demand (OHID, 2021).
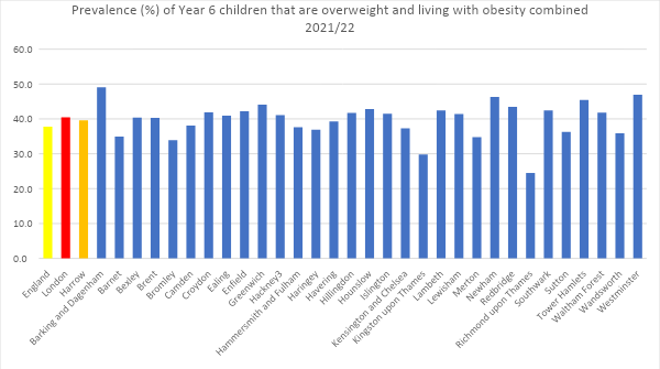
Childhood obesity
Childhood obesity and tooth decay are two diseases that are both public health problems and share a common risk factor – increased sugar consumption, so initiatives targeted at reducing sugar consumption may also result in reducing childhood obesity.
For the 2021/22 year, 19.4% of children in reception (aged 4-5 years), in Harrow were overweight and living with obesity in Harrow, this is lower than the national average for England (22.3%) and the average for London (21.9%). Whereas 40% of children in Year 6 (aged 10-11 years), were overweight and living with obesity in Harrow, this is higher than the national average (37.8%), but lower than the average for London (40.4%).
The prevalence of reception (aged 4-5 years) and Year 6 (aged 10-11 years) children that are overweight and living with obesity combined for 2021/22 was taken as part of the National Child Measurement Programme, which covered children across all mainstream state-maintained schools in England.
Figure 6: Prevalence (%) of reception children (ages 4-5 years) that are overweight and living with obesity combined by Local Authority, London (2021/22 school year)
Source: National Child Measurement Programme, England, 2021/22 school year, NHS Digital
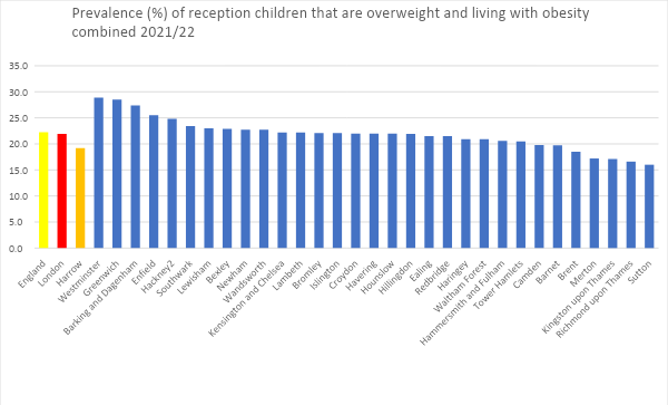
Figure 7: Prevalence (%) of Year 6 (aged 10-11 years) children that are overweight and living with obesity combined 2021/22 in the National Child Measurement Programme, England, 2021/22 school year by Local Authority, London. Source: National Child Measurement Programme, England, 2021/22 school year, NHS Digital
Oral health promotion service
Public health commissioned the Whittington NHS trust to deliver oral health promotion in Harrow from April 2021. Based on the evidence base on what works well to prevent tooth decay, the oral health promotion is based on the following key actions:
- Distribution of toothbrushes and toothpaste
- Training of the wider workforce
- Supporting the implementation of healthy food and snack policies in early years settings and schools
- Identification of an oral health champion in settings
- Promoting access to dental services
- Health education sessions with parents
- Supervised toothbrushing in schools


